Martin J. London, M.D., Professor in Residence, Anesthesia
Monitoring
Neuro Monitoring: Bispectral Index ("BIS")
BIS monitoring of anesthetic depth has gotten a lot of research and clinical attention recently, along with the topic of recall under anesthesia. It's a bit controversial just how common recall is in cardiac anesthesia with some early publications suggesting it is, while other later ones suggest it isn't. In the "old days" of high dose narcotic (in which the prevailing wisdom was that volatile agents were contraindicated), there were cases due to high opioid doses with too little benzodiazepines. In the new era of "Fast Tracking" in which volatile agents are welcomed with open arms and high doses of opioids are now considered contraindicated, this is probably less of an issue despite the claim that Fast Tracking employs "Light Anesthesia". But recall can happen even in the best done anesthestic and there are clearly several types of operations and time periods in them where certain patients may be at risk. For example, for a young otherwise healthy patient undergoing heart transplantation separation from CPB can be a particularly dangerous time as the patient is now rewarmed but the new heart may not be generating much output. In fact, the rewarming period (or termination from CPB with any temperature management strategy) can be dicey in any patient. More on this important topic later.
I've been using BIS monitoring in all of my pump cases for nearly 2 years now and think it is a major advance. Its by no means perfect and in most ways simply confirms what I had been doing all along. But its fun to use, helpful and clearly is the future of anesthetic practice (no matter what the pundits say about its increased cost per case).
Despite a slew of clinical publications (many funded by Aspect the makers of the BIS) regarding its clinical efficacy, there is very little available on the technical aspects (what's under the hood) and on intraoperative EEG monitoring in general that's easily understood by "we the people". However, our own Ira Rampil has tackled this in a recent review in Anesthesiology and it's well worth reading (hey e-mail those questions to Ira!).
The Aspect Medical Systems website has some information of educational value but frankly, I'd like to see more technical and didactic information on EEG in general. In their defense, the FDA does place some restrictions on them in this area, but..... Anyway, I'd recommend a trip there to check it out. (UPDATE: This site is now undergoing a major overhaul with lots more didactic material including a slide presentation!).
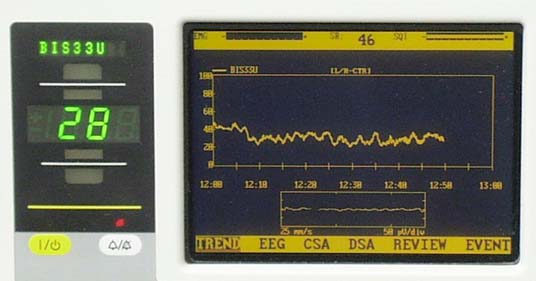
I've included a picture of the BIS in action in the heart room with a patient on bypass below. Thats the usual range most patients settle into during moderate hypothermic CPB in my experience. Shown is the older monitor (A-1050) which in most centers has been replaced with smaller, very portable, more cool, blue box (A-2000).

Here's a close-up. Notice the good quality signal as indicated by the SQI bar on the top right and the absence of EMG noise on the top left bar.
Esophageal Doppler Cardiac Output Monitoring
Deltex is agressively marketing a noninvasive doppler cardiac output monitor that in contrast to older versions (several companies have unsuccessfully marketed generations of this device for well over a decade now) appears to work! I'm not experienced enough with it to give a totally educated opinion on its accuracy, but the literature seems to support that it works fairly well. The biggest problem with the older devices was dealing with the angle at which the blood flows in relation to the doppler transducer. Recall that ideally you need to be exactly parallel to flow and the further off axis you go, the less accurate the velocity measurement is. They claim to have addressed this issue successfully. However, they haven't addressed some of my concerns about artifacts from the thoracic aorta in old folks who have lots of atherosclerosis! Really need a good TEE -EDM correlation study for that. Their site has lots of information (although just like any commercial site, info must be taken with a grain of salt!), including a nice description of the waveforms and how they are analyzed. I think this technology will spread and all anesthesiologists should be familiar with doppler techniques.


